What Is a Thoracentesis?
A thoracentesis is a procedure that removes excess fluid from the pleural space called a pleural effusion. This space is between the outside surface of the lungs and the chest wall. A catheter (a long, thin, hollow plastic tube) is inserted into the pleural space to obtain the pleural fluid. A sample of fluid may be obtained for testing to help determine the cause. Or, if you are having symptoms such as trouble breathing, it may also be done to drain the excess fluid to improve symptoms.
Before the Thoracentesis Procedure
- No food or liquids for 2 hours prior to the procedure. However, you may take all regular medications as scheduled with small sips of water.
- It is required that you arrange for a relative or friend to drive you home after the procedure.
- Report any medications you are taking to the radiology nurse, including “blood thinners”, such as aspirin, Plavix, Lovenox, Coumadin, Pradaxa, Xarelto, or Eliquis. Your physician may advise you to stop taking a “blood thinner” for a specific period of time before your procedure.
- If you are taking Coumadin or Heparin, or you have known or suspected liver disease, your blood will be tested to determine if your blood clots normally.
- Report any allergies to the radiology nurse, especially those to local anesthetic medications.
During the Thoracentesis
- You will be positioned sitting up on the ultrasound table and images will be taken to locate the site of the excess fluid inside your chest and decide where to insert the catheter.
- The skin of the chest is cleaned with an antiseptic solution and the area is covered with a large sterile sheet.
- You will feel a slight pin prick when the local anesthetic (numbing medicine) is injected in the skin.
- The doctor then carefully inserts the catheter through the skin and in between two ribs into the pleural space. The catheter will fill with fluid. A tube may be attached to the catheter so that all of the excess fluid can be drained.
- Once the fluid is drained, the catheter is removed.
- A chest x-ray will be performed after the thoracentesis to detect any complications.
Potential Risks and Complications
- Bleeding at the procedure site
- Infection at the procedure site
- Injury to an adjacent nerve, blood vessel, or muscle
- Fast drop in blood pressure
- A pneumothorax or a partial collapse of the lung may occur
- Fluid in the lung may occur if too much fluid is removed
Why Might a Person Need Thoracentesis?
During thoracentesis, our doctors remove fluids from the pleural space, which is he space between your lungs and your chest wall. A normal amount of fluid in this space is 4 teaspoons. If that amount goes up, it’s called pleural effusion, and this puts extra pressure on your lungs, making it hard to breathe.
At Summit Healthcare, we perform thoracentesis for people with pleural effusion to either improve their breathing or to help with a diagnosis. According to the American Thoracic Society, these are the most common reasons for this procedure:
- To diagnose the cause of new pleural effusion
- To improve patient comfort
- To diagnose cancer or improve cancer symptoms
- To diagnose a suspected infection
What Conditions Can Cause Fluid Build-Up?
- Congestive heart failure
- An area of pus in the pleural space
- Blood clot in the lung
- Cancer
- High blood pressure in the lung blood vessels
- Liver failure
- Pneumonia
- Reactions to medication
- Tuberculosis
- Viral, fungal, or bacterial infections
Can Anyone Not Have Thoracentesis?
Some people may not be able to safely undergo these procedures. Although not absolutely eliminated as candidates, people with these characteristics are unlikely to qualify for thoracentesis:
- Cannot be safely repositioned
- Have bleeding disorders
- Are taking blood thinners
- May have scarring from recent lung surgery
- Have other conditions that could create complications
What Are the Risks Involved with Thoracentesis?
These are safe procedures, and side effects are rare. Possible risks include:
- Pain
- Bleeding
- Bruising
- Air accumulation pushing on the lung, causing collapse
- Infection
At Summit Healthcare, we use ultrasound guidance for these procedures, and this dramatically lowers the risk of complications.
What Do Normal Results Look Like?
A normal amount of fluid in the pleural space is 4 teaspoons. That is the amount we seek when we remove the excess fluid that has accumulated.
When we remove the excess fluid in thoracentesis, we test it to figure out the reason behind the build-up. In over 90 percent of cases analysis of the removed pleural fluids yields clinically useful information. The most common cause is congestive heart failure, which is when your heart doesn’t properly pump out blood to your body.
The fluid removed is either exudate or transudate, and this distinction helps pinpoint the cause of the build-up. Exudate is defined as pleural fluid that filters from the circulatory system into lesions or areas of inflammation. Exudate results point to infection, cancer, endocrine disorders, lymphatic disorders, and other causes.
Transudate is defined as pleural fluid to serum total protein ratio of less than 0.5. These results point to causes such as congestive heart failure, cirrhosis of the liver, peritoneal dialysis, nephrotic syndrome, and other causes.
What Is the Fluid that Is Removed Tested For?
Call your doctor if you have any of the following:
- Signs of infection at the procedure site, such as redness, swelling, or a fever.
- Coughing up blood
- Bleeding from the procedure site.
- Worsening, severe pain near the procedure site.
- More than a small amount of fluid leakage from the puncture site.
- Fainting or feeling lightheaded.
If you develop shortness of breath or chest pain that is not usual for you, return to the Emergency Department immediately.
Contact us Today!
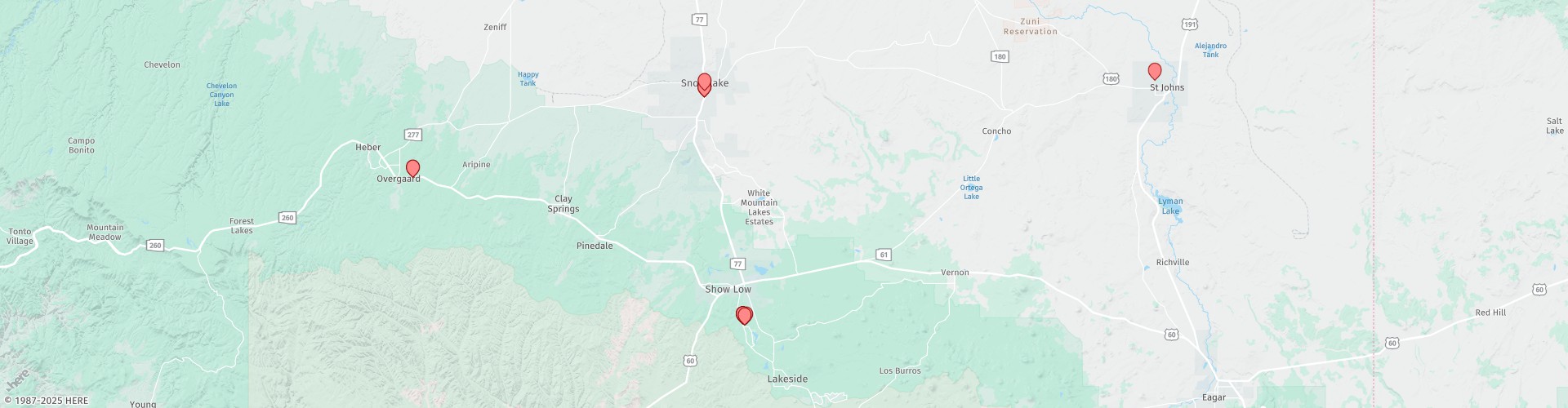
If any further questions or complications arise and you do not know what to do, please call the radiology department at Summit Healthcare at (928) 537-4375, ext. 6549. For questions after hours please ask for ext. 6332.