Summit Healthcare Provides Stroke Telemedicine
Stroke is the third-leading cause of death and foremost cause of disability. When brain cells die during a stroke, abilities like speech, movement and memory can be lost. Getting a proper diagnosis and rapid treatment improves a patient’s outcome dramatically. Every minute counts to preserve optimum brain function.
Summit Healthcare ensure that stroke victims will have immediate access to an assessment by a board-certified neurologist who specializes in stroke care. Within minutes of arriving at Summit Healthcare’s Emergency Department, the patient is assessed by an Emergency Department physician and receives a CT scan to determine whether he or she is having a stroke, and if so, what is causing the stroke – a blood clot or bleeding in the brain. The CT results are given to the physicians in the Emergency Department.
The Telestroke unit – a high-definition, large-screen computer monitor with a mobile camera – is rolled next to the patient’s bed, allowing a neurologist to become an active member of the healthcare team through the unit’s real-time two-way video conferencing. Working with the physicians in Summit Healthcare’s Emergency Department, the neurologist uses the camera and monitor to perform a thorough neurological assessment of the patient, as well as interaction with Summit Healthcare physicians and nurses. Most importantly, the neurologist helps determine if the patient is a candidate for t-PA, the clot-busting drug that improves recovery in strokes caused by blocked vessels. This drug must be administered within several hours of the onset of the stroke to be effective.
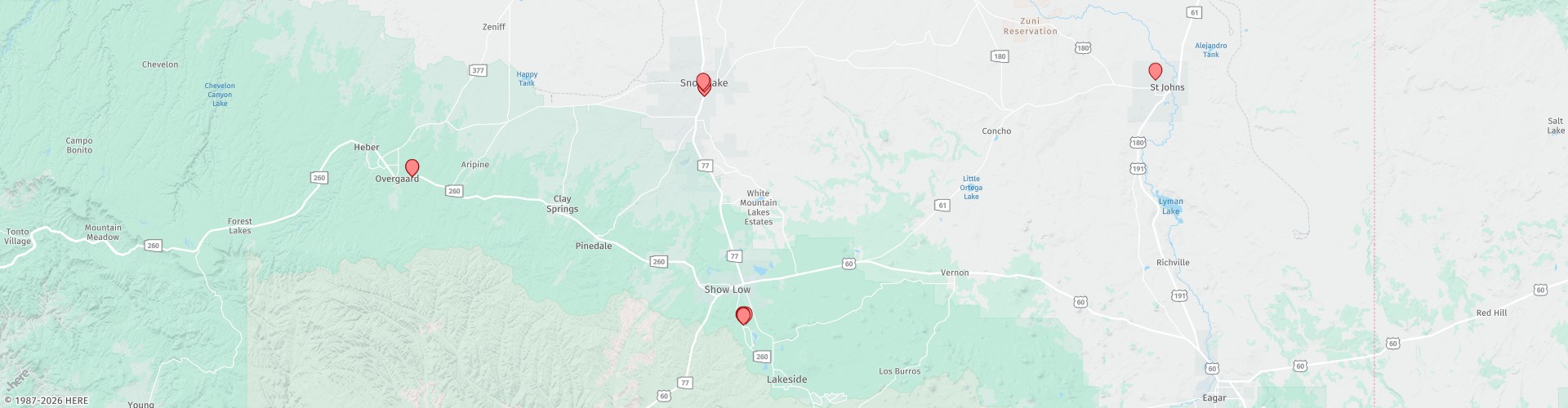
Current data shows that only 55 percent of Americans live within an hour’s drive of an acute-care stroke facility that can provide this intervention. In the White Mountains, we are a three-hour drive from an acute-care stroke facility.
In stroke telemedicine, a neurologist who has training in blood vessel conditions (vascular neurologist) at the hub consults with doctors and people who’ve had acute strokes at the remote sites (spokes). In stroke telemedicine many people work together, including a program manager, a clinical coordinator, vascular neurologists, neurosurgeons and endovascular surgical radiologists at the hub site, and emergency medicine doctors and other staff at the spoke site. Radiology technicians, informational technology staff, researchers, nurses, nurse practitioners and other staff also are critical in stroke telemedicine.
F.A.S.T.
Use the F.A.S.T. method for recognizing and responding to stroke symptoms:
F = FACE When smiling, does one side of the face droop?
A = ARMS When raising both arms, does one arm drift downward?
S = SPEECH Does the speech sound slurred or strange?
T = TIME If you observe any of these signs, it’s time to call 911.
Stroke symptoms include:
- SUDDEN numbness or weakness of face, arm or leg – especially on one side of the body.
- SUDDEN confusion, trouble speaking or understanding.
- SUDDEN trouble seeing in one or both eyes.
- SUDDEN trouble walking, dizziness, loss of balance or coordination.
- SUDDEN severe headache with no known cause.
For more information, visit www.stroke.org